The engine for growth is patient perceptions. The engine for efficiency is process improvement.1 (p. 13)
— Fred Lee
Today I’m stepping back from the communication in healthcare series, and circling back on leadership in healthcare.
When we think of relationships in our personal lives, the thought is not associated, at least one would hope, with an eye toward financial gain. Relationship-based civil leadership is based on the relatively straightforward belief that the effective relationship is, by itself, a valuable intrinsic reward. In health care, a culture suffused in relationship-based civil leadership benefit the organization with quality and safety and satisfaction levels unachievable in the business-as-usual environments.
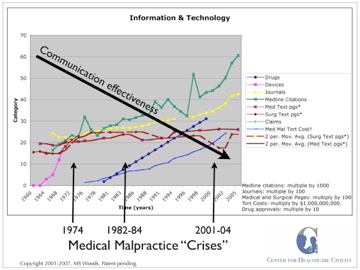
A closer look at the evolution of the medical culture over the past 30 years and the extrinsic financial motivations of today that systematically replaced our forefather’s intrinsic motivations provides us with a contrast so bright that the need for relationship-based civil leadership as a critical focus in health care culture is undeniable.
This post highlights some critical barriers to gaining broad commitment to efforts at infusing relationship-based civil leadership in health care organizations today. I would suggest that the intent of health care providers in doing what they do is important to the topic of both relationships and civility.
Confusing Money and Motivation
What is our motivation as health care providers? Is everything we do something that must be paid for? Is compensation the driver of our being? The concept of non-monetary value is something many in health care have never learned—or perhaps more accurately, we have un-learned it. Non-monetary value is something or some activity that one derives some form of gratification from that is not based upon the amount of money it either generates for the individual, or requires an individual to pay.
My thoughts on this topic emanate from the brilliance of Dee Hock. I wish I had even a reflected twinkle of the amount of brilliance this man has, but in the absence of my ability to be original along these lines, I am going to rely on Mr. Hock. In his book Birth of the Chaordic Age, he writes a great deal about value and community:2 (p. 42)
One concept…I have puzzled over is an ancient, fundamental idea, the idea of community. The essence of community, its very heart and soul, is the nonmonetary exchange of value; things we do and share because we care for others, and for the good of the place. Community is composed of that which we don’t attempt to measure, for which we keep no record and ask no recompense. Most are things we cannot measure no matter how hard we try. Since they can’t be measured, they can’t be denominated in dollars, or barrels of oil, or bushels of corn—such things as respect, tolerance, love, trust, beauty—the supply of which is unbounded and unlimited. The nonmonetary exchange of value does not arise solely from altruistic motives. It arises from deep, intuitive, often subconscious understanding that self-interest is inseparably connected with community interest; that the individual good is inseparable from the good of the whole; that in some way, often beyond our understanding, all things are, at one and the same time, independent, interdependent, and intradependent—that the singular “one” is simultaneously the plural “one.” (my emphasis)
Our society has become extremely skilled at monetizing everything. We hear the statements suggesting this truism everyday: “For enough money, you can have anything.” “People will do anything if they are rewarded appropriately.” “I’m not paid enough to do that.” I could go on, but the reader has probably already generated several more of these examples in their own head. Think about how we speak about time: we earn it, spend it, and save it! “Time is money.”
Hock continues:2 (p. 43)
Community is not about profit. It is about benefit. We confuse them at our peril. When we attempt to monetize all value, we methodically disconnect people and destroy community. (my emphasis)
The nonmonetary exchange of value is the most effective, constructive system ever devised. Evolution and nature have been perfecting it for thousands of millennia. It requires no currency, contracts, government, laws, courts, police, economists, lawyers, accountants. It does not require anointed or certified experts at all. It requires only ordinary, caring people.
What health care provider—whether physician, nurse, or technician—and what health care consumer, does not immediately understand the relevance to Hock’s insight as it relates to medicine? There is perhaps no profession where “the monetization of value” has been more misguided and abused than medicine. We—medicine and society—have put virtually an infinite number of price tags on life and health. I, as a health care consumer, value my health so highly that I will, in fact, pay large portions of my income to maintain it, or correct problems that arise. The question is “Should I have to?” A weightier question is, however, for me as the health care provider: “Is this the way it should be?” Should everything I do—every bandage I change, every conversation I have or email I exchange with a patient, every waking moment I spend at work—be something that I must be paid for? Everything that used to fall under the concept of caring now has a DRG, CPT or ICD code so we can submit a bill.
In his book Healing the Wounds, David Hilfiker has an entire chapter entitled Money.3. (p. 183) The final paragraph of the chapter reads:
Like the medieval monastic practitioners, many (I think even most) of us physicians entered medicine with the desire to serve our patients, to be altruistic healers sacrificing ourselves for their good. Clearly, even the servant should be paid for working, so there is nothing contradictory between some remuneration and our calling. Yet as the profession has become wealthier and wealthier, a contradiction has arisen. As we physicians accumulate wealth, as we earn more than we really need, we become entrepreneurs and can no longer hang on to our perception of ourselves as servants. Yet we are not willing to let it go either, to embrace the Hippocratic ideal of self-interest. So money becomes for us the hub of a very serious contradiction. At some hardly conscious level, my income proved paradoxically to be little more than an additional drain on my energies. (Author’s emphasis)
The concepts of nonmonetary and monetary lead me to a discussion of intrinsic vs. extrinsic motivation as it relates to the practice of medicine. Let’s define intrinsic motivation as an activity an individual does simply because they enjoy it or derive some level of personal gratification simply because they are able to do it… enjoyment of the work or an activity for its own sake. On the other hand, extrinsic motivation is essentially induced behavior: “If you do this, you’ll get that.” The idea of extrinsic motivation is, that, if a positive reward is given out for a task, it will lead one to continue wanting to do the task, to keep getting the reward. It is, in essence, a method of controlling behavior, and is, in reality, no different than the promise of punishment if one does not do something.4 In other words, the promise of a reward could be reworded to say, “If you don’t do that, you won’t get this,” which is, in essence, a form a punishment. Think of pay-for-performance—is this not the perfect example of extrinsic motivation?
Up next in the Leadership Series: A Chasm of Disconnect: Community, Motivation, and the Patient: Part Two
All content from Civil Leadership, by Michael S. Woods. © 2007. All rights reserved.
References
- Lee. F: If Disney Ran Your Hospital. Bozeman, MT: Second River Healthcare Press, 2004.
- Hock, D: Birth of the chaordic age. San Francisco: Berrett-Koehler Publishers, 1999.
- Hilfiker, D. Healing the wounds. New York, Pantheon Books, 1985.
- Kohn, A: Punished by Rewards. New York: Houghton Mifflin, 1993.